52 year old with shortness of breath since one day
This is an online E logbook to discuss our patient’s de-identified health data shared after taking his signed informed consent.
Here we discuss our individual patient’s problems through series of inputs from the global online community of experts with an aim to solve those patient’s clinical problems with collective current best evidence-based inputs.
This E-logbook reflects my patient-centered online learning portfolio.
Preity Yarlagadda
Roll no - 145
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
CASE : A 52yr old male came to the OPD with the chief complaints of decreased urine output and shortness of breath at rest since one day.
HOPI :
- Patient was apparently asymptomatic 2 days ago when he developed Shortness of breath Grade II (on exertion) which progressed to Grade IV (at rest) for which he visited local RMP and was referred to our hospital.
- Patient also complains of decreased urine output since 2 days and Anuria since morning.
- No H/o Fever, cold, burning micturition, chest pain.
- No H/o Palpitations, giddiness, sweating.
- H/o Shortness of breath (Grade II i.e SOB on exertion) 1yr ago for which he visited the local hospital and was diagnosed to be Hypertensive (On medication).
- H/o HTN since 1yr.
- H/o Facial puffiness On and Off since 2-3yrs.
- H/o Surgery for Inguinal hernia 10yrs ago. Patient was fine after the surgery, but had On and Off pain at surgical site which aggravated since 3yrs.
- Not a K/C/O DM, TB, CVA, CAD, Epilepsy, Asthma.
- Appetite : Normal
- Diet : Mixed
- Bowel and bladder movements : H/o Constipation since 2 days
- Addictions : Occasional alcoholic, H/o NSAID abuse since 3yrs, non-smoker.
No significant Family history
GENERAL EXAMINATION :
The patient was conscious, coherent and cooperative, sitting comfortably on the bed.
He is well oriented to time, place and person.
He is moderately built and well nourished.
VITALS :
Temperature - Afebrile
Pulse - 100 bpm
BP - 80/60 mmHg
Respiratory rate - 16 cpm
No Pallor, Icterus, Clubbing, Lymphadenopathy, Edema
SYSTEMIC EXAMINATION :
CVS - S1, S2 heard, No Murmurs
RS - Elliptical and bilaterally symmetrical chest
Both sides moving equally with respiration
Bilateral air entry - Present
Normal vesicular breath sounds
CNS - No abnormal defects, Reflexes can be elicited
Per Abdomen - Soft and Non tender
Bowel sounds can be heard.
INVESTIGATIONS :
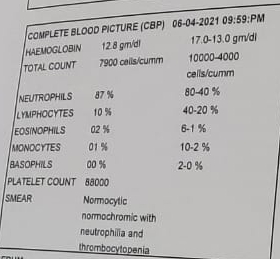
1. Complete blood picture
* Hemoglobin - 12.8 gm/dl
* Neutrophils - 87%
* Platelets - 88000
2. Complete urine examination
* Albumin +++
3. Renal function test
* Urea - 198mg/dl
* Creatinine - 5.4mg/dl
* Uric acid - 11.9mg/dl
* Phosphorus - 5.6mg/dl
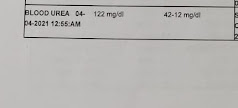
4. Blood urea
* Blood Urea - 122mg/dl
5. Serum creatinine
* Serum Creatinine - 3.2mg/dl
6. Arterial blood gas
7. Liver function test
* Total Bilirubin - 2.96mg/dl
* Direct Bilirubin - 1.93mg/dl
* SGOT - 476 IU/L
* SGPT - 551 IU/L
* Alkaline Phosphate - 172 IU/L
8. CT pulmonary angiogram
* Dilated Main Pulmonary Artery and Left Pulmonary Arteries.
* No evidence of Pulmonary Arterial Embolism.
*Thrombi noted in Left Atrial Appendages and Left atrium
9. 2D Echo
* Dilated All chambers
* Global Hypokinesia
* Severe LV dysfunction (EF = 28) (Moderate to severe eccentric TRF positive)
* IVC dilated 2.15 cms
PROVISIONAL DIAGNOSIS :
CCF at Presentation ( Resolved )
AF with RVR
Biatrial Thrombus with ASD (6-7mm) with PAH
Cardio Renal Syndrome 4
Denovo DM 2
COURSE IN HOSPITAL :
On the day of admission -
* INJ. Dobutamine 3.6ml/hr was given to maintain the falling BP up to a MAP of 55 mmHg.
On Day 3 -
* ECG showed Irregular rhythm and he was started on TAB. Digoxin 0.25mg OD 5/7 and INJ. Unfractionated Heparin 5000 IU TID.
* As patient's D DIMER was high, Anti coagulants were started and planned for CPTA.
On Day 4 -
* Patient was started on TAB. Carvediol 3.125mg BD
On Day 5 -
* Patient's Serum Creatinine and Serum Urea were increased after CPTA.
* Nephrology opinion was taken in view of Contrast Induced Nephropathy.
On Day 6 -
* Patient was started on INJ. Unfractionated Heparin Infusion @5ml/hr and TAB. Acetyl cysteine 600mg PO TID.
* Daily monitoring of APTT, PT, INR and RFT was done.
On Day 7 -
* TAB. Acitrom 2mg OD was started.
On Day 8 -
* The Infusion of Heparin was increased to 7ml/hr and it was stopped after attaining the APTT of >70secs, PT of 23secs and INR of 2.3.
Other medications used during the course in hospital -
1. TAB. Cardivas3.125mg PO/BD
2. TAB. Dytor 10mg PO/OD
3. TAB Pan D 40mg PO/OD
4. TAB. Taxim 200mg PO/OD
5. INJ. Thiamine 100mg in 50ml NS IV/TID
6. INJ. HAI S.C 8U-8U-6U
** As patient symptomatically improved during stay in the hospital, he was Discharged on request, on 12-4-21.**
ADVICE AT DISCHARGE :
1. TAB. Dytor 10mg PO/OD
2. TAB. Acitrom 2mg PO/OD
3. TAB. Cardivas 3.125mg PO/BD
4. INJ. HAI S/C 6U-6U-4U
5.TAB. Digoxin 0.25mg OD 5/7 except Saturday and Sunday
6. Hypoglycemia symptoms explained
7. Watch for any bleeding manifestations like Petechiae, Bleeding gums.
8. PT, INR, APTT after 15 days and Review sos.
FOLLOW UP on 15-05021 :
* The patient is taking medication regularly.
* The patient has regular bowel and bladder movements, normal appetite and sleep pattern.
* The patient has no Shortness of breath, Hypoglycemia symptoms or Bleeding manifestations.
* The patient is yet to get the recommended tests done.
DISCUSSION :
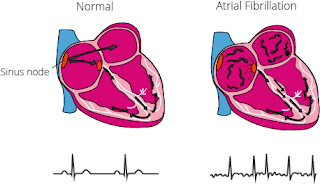
Atrial Fibrillation and Biatrial Thrombosis :
Pathogenesis :
Loss of Atrial contraction and Left atrial dilatation causes stasis of blood in the LA and may lead to Thrombus formation in the Left Atrial Appendage. This predisposes patients to stroke and other forms of systemic embolism.
Clinical Features of A-Fib :
Palpitations, breathlessness, fatigue, lightheadedness and chest pain
Common Causes of A-Fib :
Coronary heart disease, Hypertension, Valvular heart disease, Cardiomyopathy, Alcohol, Chest infection, etc.
Management :Depends of whether Atrial Fibrillation is Paroxysmal or Persistent
1. If Paroxysmal Atrial Fibrillation -
- Beta-blockers are used as first line therapy since they reduce the ectopic firing that initiates the arrhythmia. They are particularly useful in patients associated with Coronary artery disease, Hypertension and Cardiac failure.
- Class 1c drugs such as Propafenone, flecainide are also effective.
- Ablation for AF is an attractive treatment when drugs are ineffective or poorly tolerated.
- Rhythm control - IV Flecainide can be used for pharmacological cardioversion and will restore sinus rhythm. (IV Amiodarone if any heart disease present)
- Rate control - Digoxin, Beta blockers, CCBs like Diltiazem or Verapamil reduce the ventricular rate by slowing AV conduction.
- Thromboprophylaxis - Patients undergoing cardioversion to restore sinus rhythm require temporary anticoagulation to reduce the risk of systemic embolus. Warfarin, direct acting anti-coagulants like factor Xa and direct thrombin inhibitors can be used.
Thrombus Management
- If LAA thrombus was diagnosed in previously non-anticoagulated patients then most prevalent first-line treatment is NOCA (Novel Oral Anticoagulants)
- The patient is advised to look out for bleeding manifestations like petechiae. bleeding gums etc.
- The patient is asked to regularly monitor APTT, PT and INR.













Good Blog
ReplyDelete