Long case for Final practicals - 75 year old female with vomitings and giddiness
This is an E log book to discuss our patient's de-identified health data shared after taking his guardian's signed informed consent. Here we discuss our individual patient problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable comments in comment box are most welcomed.
I have been given this case to solve in an attempt to understand the topic of "Patient clinical data analysis" to develop my cmpetancy i reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
HALL TICKET NO - 1701006199
CASE :
A 75 years old female, home maker by occupation, resident of nalgonda was bought to the casuality with chief complaints of
- vomitings since 1 day
- giddiness since 1 day.
HISTORY OF PRESENTING ILLNESS :
• Patient is a known case of diabetes mellitus and hypertension since 6 years.
•She was apparently asymptomatic 6 years back.
- Later she had complaints of headache, generalized weakness for which she was taken to a hospital and there she was diagnosed with diabetes mellitus and hypertension and prescribed on oral medication. From then she was on regular medication.
• Patient did not use oral hypoglycemics and anti- hypertensives for the past 4 days as she went to relatives house.
• Patient presented with 2-3 episodes of vomitings, non- bilious and non - projectile followed which she developed giddiness.
- Contents of the vomitus are food and it is not foul smelling.
- No history of fever or pain abdomen.
- She was taken to a local hospital where it was found out that her GRBS is 394mg/dL and ketone bodies were positive and referred to our hospital.
• No history of shortness of breath, chest pain, palpitations.
PAST HISTORY :
- She is a known case of diabetes mellitus and hypertension since 6 years.
- No history of Tuberculosis, cardiovascular disease.
- Surgical history - history of cataract surgery 3years back in one eye and 2 years back in the other eye.
- Diet - mixed
- Appetite - normal
- Sleep - adequate
- Bowel and bladder movements - regular
- Addictions - chutta smoking for 10years , 3 chutta per day and stopped 5 years back.
- No allergies
- Not significant
- Attained menopause
- 8 children - 4 boys and 4 girls
- Patient was examined in a well lit room after taking informed consent.
- She was conscious, coherent and cooperative. Moderately built and we'll nourished.
- Oriented to time, place and person.
- Pallor - present
- Icterus - absent
- Cyanosis - absent
- Clubbing - absent
- Generalized lymphadenopathy - absent
- Bilateral pedal edema - absent
VITALS :
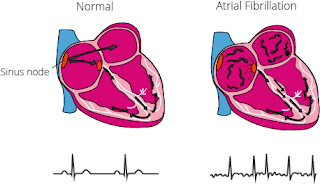
- Pulse - 96 beats per minute, irregularly irregular in rhythm, no radio-radial delay, no radio- femoral delay.
- Blood pressure - 230/100 mm of hg measured in left arm in supine position
- Respiratory rate - 17 cycles per minute
- Temperature - Afebrile
- GRBS - 393 mg/dL
- INSPECTION :- No visible pulsations, no visible apex beat, no visible scars.
- PALPATION :- Apex beat felt
- AUSCULATION :- Mitral area, tricuspid area, pulmonary area, aortic area - S1, S2 heard.
- Higher mental functions - Normal
- Cranial never functions - Normal
- Sensory system - Sensitive
- Motor system Right Left
- Cerebellar system - Intact
- INSPECTION - No tracheal deviation, Chest bilaterally symmetrical. Thoraco abdominal type of respiration. No dilated veins, pulsations, scars or sinuses.
- PALPATION - No tracheal deviation, normal vocal fremitus on both sides.
- PERCUSSION - Resonant in all areas.
- AUSCULATION - Normal vesicular breath sounds, bilateral air entry present.
- INSPECTION - Abdominal distension is present, umbilicus is normal. All quadrants are moving equally with respiration. No visible scars, sinuses, pulsations, engorged veins.
- PALPATION - No local rise of temperature or tenderness in all quadrants. No organomegaly.
- PERCUSSION - No shifting dullness
- AUSCULATION - Bowel sounds and heard, no bruit.
INVESTIGATIONS :
- Hemoglobin - 11.3mg/dl
- RBC - 4.47 million/cumm
- TLC - 8900 cells/cumm
- Neutrophils - 80%
- Lymphocytes - 13%
- Eosinophils - 02%
- Monocytes - 05%
- PCV - 33.7 volume%
- MCV - 75.4 fl
- MCH - 25.3 pg
- MCHC - 33.5%
- Platelets - 2.56 lakhs/cumm
- Blood picture - Normocytic normochromic
Complete urine examination -
- Colour - Pale yellow
- Apperance - Clear
- Reaction - Acidic
- Specific gravity - 1.010
- Albumin - 2+
- Sugar - 4+
- Bile salts and pigments - Nil
- Pus cells - 3-6/hpf
- Epithelial cells - 2-4/hpf
- RBC - Nil
- Casts - Nil
- POSITIVE on 09-06-22
- NEGATIVE on 11-06-22
- pH - 7.44
- pCO2 - 30.6mmHg
- pO2 - 71.4mmHg
- HCO3 - 22.6mmol/L
- O2 saturation - 93.8%
- Sodium - 139mEq/L (09-06)
- Potassium - 3.3mEq/L (09-06)
- Chloride - 98mEq/L (09-06)
Blood urea - 26 mg/dl
- Total bilirubin - 0.74mg/dl
- Direct bilirubin - 0.18mg/dl
- Aspartate transaminase - 29 IU/L
- Alkaline phosphate - 143 IU/L
- Alanine transaminase - 11IU/L
- Total proteins - 7.7g/dl
- Albumin - 4.1g/dl
- A/G ratio - 1.16
- Intra venous fluids (Normal saline or Ringers lactate ) - 100ml/hr.
- Human ACTRAPID insulin infusion - 6ml/hr.
- Tab. NICARDIA 20mg PO/stat.
- Inj. OPTINEURON - 1 ampoule in 100ml of Normal saline I.V / OD.
- Inj. ZOFER 4mg I.V/ TID.
- Hourly monitoring of GRBS, pulse, BP, RR and Temperature.
- Intra venous fluids 2 NS - 100ml/he
- Inj. Human ACTRAPID insulin infusion - 6ml/hr
- Inj. OPTINEURON - 1Ampoule in 100ml NS I.V OD
- Tab. TELMA AM 40/5 mg PO OD
- Inj. ZOFER 4mg I.V TID
- Monitoring GRBS, BP, RR, PR.
- Strict input output charting
- Intravenous fluids 2 NS - 75ml/he
- Inj. Human ACTRAPID insulin 10/10/10 and NPH 8/-/8, strict GRBS monitoring
- Inj. OPTINEURON 1 ampoule in NS I.V OD
- Inj. ZOFER 4mg I.V TID
- Tab. CINOD-T (40/10) mg PO OD
- BP 2hrly charting
- Strict input /output charting
- Inj. Human ACTRAPID insulin 12/12/12 and NPH 10/-/10, strict GRBS monitoring
- Inj. OPTINEURON 1 ampoule in NS I.V OD
- Inj. ZOFER 4mg I.V TID
- Tab. CINOD-T (40/10) mg PO OD
- BP 2hrly charting
- Strict input /output charting
- Inj. Human ACTRAPID insulin 12/12/12 and NPH 10/-/10, strict GRBS monitoring
- Inj. OPTINEURON 1 ampoule in NS I.V OD
- Inj. ZOFER 4mg I.V TID
- Tab. CINOD-T (40/10) mg PO OD
- BP 2hrly charting
- Strict input /output charting
- Inj. Human ACTRAPID insulin 10/10/8 and NPH 8/-/6, strict GRBS monitoring
- Inj. OPTINEURON 1 ampoule in NS I.V OD
- Inj. ZOFER 4mg I.V TID
- Tab. CINOD-T (40/10) mg PO OD
- BP 2hrly charting
- Strict input /output charting












Comments
Post a Comment