43 year old male with weakness of upper and lower limbs since 2 days
Introduction: This is an online E-log Entry Blog to discuss, understand and review the clinical scenarios and data analysis of patients so as to develop my clinical competency in comprehending clinical cases, and providing evidence-based inputs.
Note: The cases have been shared after taking consent from the patient/guardian. All names and other identifiers have been removed to secure and respect the privacy of the patient and the family.
Consent: An informed consent has been taken from the patient in the presence of the family attenders and other witnesses as well and the document has been conserved securely for future references.
CASE :
A 43 year old male presented to the casualty with complaints of
- weakness of both upper and lower limbs since 2 days.
---The patient was apparently asymptomatic 15 days ago, when he developed swelling in both lower limbs and face for which he went to Osmania hospital.
---After investigations, he was diagnosed to have End stage kidney disease.
--- 6 Sessions of dialysis was done in Osmania hospital (Done alternate days). The patient was fine after these sessions.
--- On 22-07-23, after the 7th dialysis session, the patient couldn't stand or walk but the doctor told the attenders that it was because of the long dialysis session and discharged the patient.
--- On 23-07-23, the patient still couldn't stand or walk and also had sluggish speech so the patient was taken back to Osmania hospital. The patient wasn't taken care of properly so the attenders shifted him to a private hospital in Alwal.
--- On 23-07-23, (S. creat - 7mg/dl) one session of dialysis was done in the private hospital. The patient was coherent but still couldn't move his lower limbs.
--- On 24-07-23, central line of the patient was removed as it was infected. Due to financial issues, patient was discharged from the hospital.
--- On 24-07-23, patient was brought to our casuality with weakness of both upper and lower limbs.
Past history :
- Patient is a k/c/o DM - 2 since 10 years. He was using Tab. Metformin 500mg PO/BD. Since last 15 days, patient is using Inj. Mixtard 8U ---- 6U
- Patient also has HTN (denovo) since 15 days, using Tab. Nicardia 20mg
- Patient is not a k/c/o epilepsy, cad, asthma.
- Appetite - normal
- Mixed diet;
- Regular bowel and bladder movements;
- Sleep adequate
- No known allergies,
- Alcoholic since 6 years (consumes 70-90ml 3 to 4 times a week) Stopped 2 months ago.
General examination :
Patient is drowsy, not oriented to time, place and person.
After 4 hours, the patient was oriented.
Pallor present
No signs of icterus, cyanosis, clubbing, edema, lymphadenopathy.
Vitals on admission :
BP - 90/60mmhg
PR - 100bpm
RR - 20cpm
SpO2 - 95% on RA
GRBS - 113mg/dl
Temp - 99.8 F
Systemic examination :
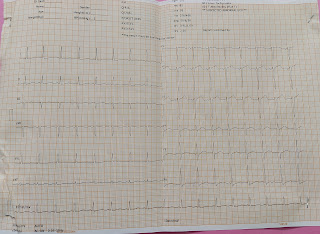
CVS - S1, S2 heard, no murmurs
RS - BAE +, NVBS heard
PA - soft, non tender
CNS -
Tone R L
UL increased increased
LL increased increased
Power - Unable to elicit
Reflexes R L
Biceps - -
Triceps - -
Supinator - -
Knee - -
Ankle - -
Plantar Extension Extension
Provisional diagnosis :
CKD with Diabetic nephropathy (Grade III)
?Sepsis
With DM - II and HTN
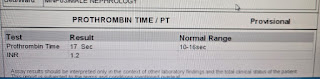
Investigations :
On 07-07-23 :
On 23-07-23 (done in the private hospital)
Serum Creatinine - 7mg/dl
Blood urea - 156mg/dl
Na + 133mmol/L
K+ 2.3mmol/L
Ca+2 7.9mg/dl
Cl- 105mmol/L
On 24-07-23 (in our hospital) :
Serum creatinine - 4.3 mg/dl
Blood urea - 67mg/dl
On 25-07-23
Treatment :





























Comments
Post a Comment