60 year old female with headache
Introduction: This is an online E-log Entry Blog to discuss, understand and review the clinical scenarios and data analysis of patients so as to develop my clinical competency in comprehending clinical cases, and providing evidence-based inputs.
Note: The cases have been shared after taking consent from the patient/guardian. All names and other identifiers have been removed to secure and respect the privacy of the patient and the family.
Consent: An informed consent has been taken from the patient in the presence of the family attenders and other witnesses as well and the document has been conserved securely for future references.
CASE :
A 60 year old female presented to the OPD with the chief complaint of
- Headache since 3 months.
HOPI : The patient was apparently asymptomatic 3 months ago, when she fell down the stairs and hit her head.
There was no visible wound, no loss of consciousness, no vomiting, no blurring of vision, no ent bleed.
The patient complaints of headache since 3 months, which is diffuse, intermittent and throbbing type, with no aggravating or relieving factors.
It is not associated with any aura, nausea or vomiting. No c/o photophobia, phonophobia.
C/o heartburn which is aggravated with spicy food and relieved after taking antacids.
No C/o sob, palpitations, chest pain.
C/O unilateral pitting edema which is pitting type and intermittent.
Past history :
K/c/o Htn since 6 months, using medication
Tab. Telma H (40/12.5)
Not a k/c/o DM, asthma, epilepsy, thyroid disorders.
Personal history :
Normal Appetite, mixed diet, regular bowel and bladder movements, adequate sleep, no known allergies, no addictions.
Family history :
Not significant
General examination :
Patient is C/C/C, well oriented to time, place and person.
No signs on pallor, cyanosis, clubbing, lymphadenopathy, edema.
Vitals on admission :
BP - 160/100mmhg
PR - 80bpm
RR - 16cpm
Temperature - 98.2 F
Spo2 - 99% on RA
GRBS - 117mg/dl
Systemic examination :
CVS - S1, S2 heard, no murmurs.
RS - BAE+ , NVBS heard
PA - Soft, non tender, no organomegaly
CNS - NFAD.
PROVISIONAL DIAGNOSIS :
TENSION HEADACHE
Investigations :
Hemogram
CUE
RBS
LFT
Serum creatinine
Blood urea
Serum Electrolytes
Serology
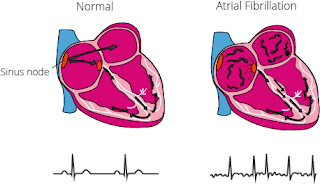
ECG
Chest Xray
2D ECHO
USG - Abdomen and pelvis









Comments
Post a Comment